
© 1998-2023 Mayo Foundation for Medical Education and Research (MFMER). It's important to determine the cause, since some underlying problems can be potentially serious. See your doctor promptly if you or your child develops unexplained or widespread petechiae. Petechiae may also be caused by noninfectious medical conditions. Petechiae may be caused by any of a number of fungal, viral and bacterial infections, including: Petechiae may result from taking some types of medications, including: Tiny petechiae of the face, neck and chest can be caused by prolonged straining during activities such as coughing, vomiting, giving birth and weightlifting. A number of things can cause this bleeding, including: Petechiae and purpura are common when the platelet count is severely low, whereas systemic symptoms, such as arthralgias or abdominal discomfort, are not present. Petechiae appear when capillaries bleed, leaking blood into the skin. Tiny blood vessels (capillaries) link the smallest parts of your arteries to the smallest parts of your veins. Petechiae are common and may indicate a number of conditions, ranging from minor to very serious. Sometimes they appear on the inner surfaces of the mouth or the eyelids.

Usually flat to the touch, petechiae don't lose color when you press on them. Petechiae (puh-TEE-kee-ee) commonly appear in clusters and may look like a rash. The bleeding causes the petechiae to appear red, brown or purple.
Pinpoint petechiae skin#
12 The rash is gravity and pressure dependent.Petechiae are pinpoint, round spots that appear on the skin as a result of bleeding. Some patients have target-like lesions, with each lesion consisting of a central punctate hemorrhage surrounded by circumferential regions of pallor and hemorrhage. 12 Some patients present with predominantly petechial lesions, some present with mainly purpuric lesions, and others present with a mixture of lesion types. It is the presenting sign in 50 percent of patients. 13 Palpable purpura is present in almost 100 percent of patients with Henoch-Schönlein purpura. Streptococcus is the most common infecting organism. 11 From 60 to 75 percent of patients with Henoch-Schönlein purpura have a history of a preceding upper respiratory tract infection. 1 The condition is twice as prevalent in males as in females.
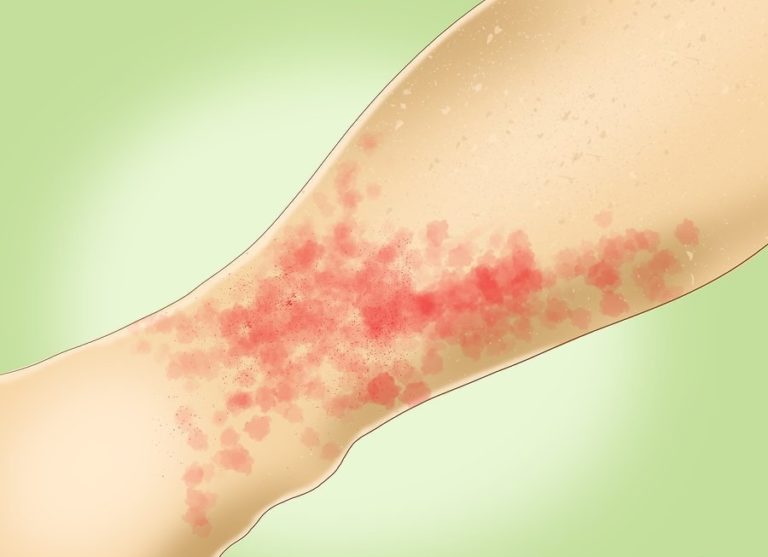
Even certain medications you take may lead to petechiae. There are many causes of petechiae, from a simple skin abrasion to a serious diagnosis like meningitis or leukemia. They are a symptom of another underlying condition. 1 Approximately 75 percent of cases occur in children between two and 11 years of age. Petechiae are small, pinpoint red dots that form a skin rash but don't itch.

11, 12 This condition is the most common form of vasculitis in children. The hallmarks are nonthrombocytopenic purpura, abdominal pain, arthritis and nephritis. Henoch-Schönlein purpura is an IgA-mediated systemic vasculitis of small blood vessels. 6 Chronic idiopathic thrombocytopenic purpura is more likely to present in teenage girls and children with underlying immune disorders. 5 Idiopathic thrombocytopenic purpura is usually a temporary disorder, with 80 to 90 percent of children recovering within six to 12 months, usually within a few weeks. Minimal splenomegaly occurs in about 5 to 10 percent of symptomatic children. Fever, lethargy, weight loss, bone pain, joint pain, pallor, lymphadenopathy and hepatosplenomegaly are characteristically absent. The peak incidence is between two and four years of age. An antecedent viral infection, especially an upper respiratory tract infection, is common.

4 The characteristic presentation is the sudden onset of bruises, purpura, mucosal hemorrhage and petechiae in a child who is otherwise in excellent health. The disorder is caused by the development of IgG autoantibodies to platelet membrane antigens as a result of an unbalanced response to an infectious agent or autoimmunity. Idiopathic (immune) thrombocytopenic purpura is by far the most common etiology of thrombocytopenia in childhood. Immune thrombocytopenia is the most frequent cause of increased platelet destruction.


 0 kommentar(er)
0 kommentar(er)
